Key Topics
- Active electrodes record the signal from the stimulated region, reference electrodes record ambient noise, and the ground electrode serves as the zero reference for the positive or negative polarity of the signal.
- Comparison of commonly used ERG active electrodes for signal amplitude (specifically signal to noise ratio) and patient comfort.
- Limited options for VEP/EOG active electrode due to placement requirements.
- Non-proprietary electrodes routinely recommended by Diagnosys.
Introduction
Currently, there are many commercially available electrodes capable of performing electrophysiology tests compliant with standards set forth by the International Society for Clinical Electrophysiology in Vision (ISCEV). Choosing which one to use can be confusing but understanding an electrode’s strengths and weaknesses will help in selecting the appropriate one for your needs.
Any electrophysiology vision function test performed on a human requires three electrodes (active, reference, and ground). For the purpose of this review, Diagnosys has grouped the electrodes into the following categories—ERG Active, VEP/EOG Active, and Reference/Ground.
A list of the published research used for this review can be found at the end of the article.
ERG Active Electrodes
The electrodes used to record the electroretinogram (ERG) active signal have been widely researched due to the need to balance electrode performance with patient safety and comfort. Both performance and comfort need to be optimized in order to obtain reliable and repeatable results.
Electrodes used to record the active ERG signal must be placed as close to the stimulated source of interest – the retina – as possible. Although an electrode on the apex of the cornea yields the largest active signal, it is also the least comfortable for the patient. Thus, the challenge is to balance signal strength with patient comfort.
Over the years, inventors have created several different electrode designs that fall into three main categories identified by where the electrode is placed—contact lens, conjunctival, and skin.
A comparison of the electrode signal strengths reveals that if the contact lens records an amplitude of 100 percent, the conjunctival electrode recording of the same ERG would be approximately 80 percent, while the skin electrode recording would be roughly somewhere between 25-35 percent. It is worth noting that although signal strength may be affected by electrode type, signal timing and waveform are largely unaffected.
In conjunction with signal strength, signal to noise ratio is a significant factor when attaining quality ERG results. Noise may be introduced into the signal by inherent electrode properties that influence connection quality, called impedance. For example, contact lens and conjunctival electrodes are placed directly on the surface of the moist eye that is inherently conductive. Skin electrodes accrue greater background noise as the signal must travel through skin before reaching the electrode.
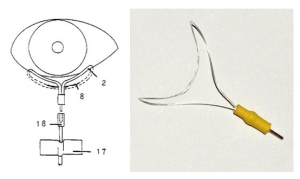
Contact lens electrodes
Contact lens electrodes generally record the largest ERG amplitudes because the active electrode is in constant contact with the cornea, encircling the apex. These electrodes hold the eye open to prevent blinking, thus many patients may find them uncomfortable or intimidating. Topical anesthesia is always used and younger patients are generally sedated.
While the lenses can be used for several hours at a time, a session of 30 minutes or less is practical for most patients (Heckenlively, 2006). Prolonged recordings increase the risk of corneal abrasions, conjunctival abrasions, and irritation from the lens moving against the cornea.
Notably, the contact lens adds a layer of material atop the cornea, which alters a patient’s refraction. Therefore, contact lens electrodes should not be used for pattern ERG (PERG).
The most common contact lens electrodes today are Hansen Ophthalmic’s Burian Allen and Fabrinal’s Jet electrode.
Burian Allen
Not sold by Diagnosys
The Burian Allen is a reusable contact lens electrode by Hansen Ophthalmic Development Laboratory. These lenses come in eight different sizes ranging from adult down to premature infant. These electrodes are hand-made and thus often require a six to twelve month wait time after placing an order.
There are two types of Burian Allen—unipolar and bipolar. A bipolar lens includes both active and reference electrodes, while a unipolar lens contains only the active electrode.

Jet electrode
D233: order here

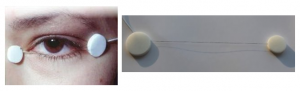
Conjunctival electrodes
Conjunctival electrodes are placed on the eye but instead of covering the cornea, they lay mostly in the conjunctiva. Researchers developed these electrodes in order to create a more patient friendly alternative to the contact lens electrode. Many clinicians consider these electrodes to be the best at optimizing both performance and comfort. Topical anesthesia is not required, but may be necessary depending on the patient. Conjunctival electrodes can be worn comfortably for longer periods of time than contact lens electrodes because their small size allows patients to blink freely.
In addition, these electrodes do not alter the patient’s refraction making them ideal for tests like pattern ERG (PERG).
Consistent placement of conjunctival electrodes is imperative in order to obtain reliable and repeatable test results. To achieve this goal, Diagnosys recommends developing a repeatable method by which the electrode is consistently placed in the same location every time a patient is tested.
Currently, the more popular conjunctival electrodes are the DTL Plus (inventors Dawson, Trick and Litzkow, US), the gold foil (inventors Carter & Hogg, UK), and the H-K Loop (inventors Hawlina and Konec, Slovenia). All three of these electrodes are unipolar.
DTL Plus Electrode
D141: order here
The single use DTL Plus improves upon the original DTL design and is commercially available from Diagnosys. Instead of one thread, the electrode is now composed of several 6cm long nylon threads coated with medical grade silver. The multi-thread design improves strength integrity so if one thread breaks, the others will still carry the electrical signal. Two small adhesive pads secure the DTL Plus at the nasal and temporal canthi. The thread drapes across the sclera usually along the lower lid. This position is known as the lower lid position (LLP). The DTL can also be placed lower into the fornix, which is known as the fornix position (FP). A recent paper studied the two placements and found that the LLP records higher amplitudes while the FP is more comfortable (Brouwer, 2020). What is most important is to choose one of the positions and ensure that the electrode remains in that position throughout the recording.This electrode excels in the area of patient comfort, reduced noise and artifact, optical quality, and low electrode impedance. It also eliminates the risk of corneal abrasions and conjunctival infections. Numerous studies have shown that the vast majority of patients prefer DTLs to any other electrode for comfort.
Gold foil electrode
Not sold by Diagnosys
The gold foil electrode is a reusable electrode made of flexible mylar-gold that is “hooked” or shaped around and under the lower eyelid. It may come into contact with the corneal-scleral junction on the midline.Although reusable, sterilizing them can be difficult and there is disagreement among researchers about whether electrodes reused more than three times produce decreased amplitudes.
H-K Loop electrode
Not sold by Diagnosys
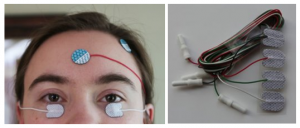
Skin Electrodes
Skin electrodes used as the active ERG electrode are placed on the skin directly beneath the eye. ERG amplitudes measured by skin electrodes are significantly less than both contact lens and conjunctival electrodes. ERGs recorded using a skin electrode are small and quite variable in amplitude because the eye-to-skin current pathway contains high and varying resistances. (Arden, 1979)
The impedance when using skin electrodes is naturally quite high. To lower the impedance, the skin beneath the electrode must be carefully scrubbed to remove all oils and dead skin cells. Larger skin electrodes require larger areas of skin to be prepped; this preparation must be done well or noise may conceal the ERG signal.
There are a variety of reusable and single use skin electrodes commercially available that can be used as the ERG active electrode. Diagnosys prefers to use a small 20×15 mm disposable sticky pad electrode because it is lightweight and doesn’t pull down the lower lid, is soft and flexible for comfort, can be repositioned if necessary, and only a small area of skin needs to be prepped.
These small disposable sticky pad electrodes are ideal for pediatric ERGs.
Regardless of which type of electrode is used—contact lens, conjunctival, or skin—reliable interpretation of ERG recordings requires comparison with electrode-specific and age-matched normative data (Heckenlively, 2006).
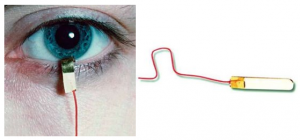
VEP and EOG Active Electrodes
The visually evoked potential (VEP) and the electrooculogram (EOG) are electrophysiology tests that require placement of the active electrode in different locations than the ERGs. There are only a few options for a VEP or EOG active electrode .
The VEP indicates the function of the entire visual pathway from the retina to area V1 of the visual cortex and primarily reflects the central retinal projection to the occipital poles in response to light stimulus. ISCEV guidelines require that recording electrodes be positioned on the scalp in accordance with anatomical landmarks. The standardized International 10/20 system measurement method should be used for exact electrode placement.
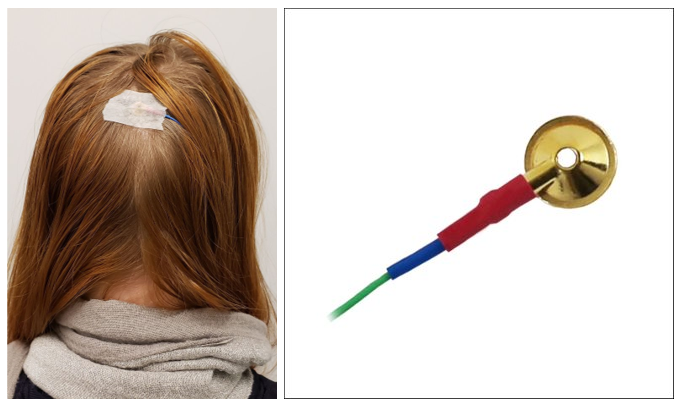
The VEP is usually recorded with small scalp electrodes composed of gold or silver, often simply called a gold cup electrode. These electrodes are reusable but there are also single usedisposable gold cup electrodes with detachable cables. A conductive paste or gel is used to maintain the bridge between the electrode and the scalp.
Sticky pad skin electrodes are impractical as an electrode on the occipital cortex unless the patient is bald because hair obscures the conductive pathway.
Gold cup electrode
D133: order here
The EOG measures the standing eye potential to document retinal pigment epithelium function. This test requires the use of small skin electrodes placed next to the nasal and temporal canthi. It is necessary to use small skin electrodes like a gold cup or a small sticky pad in order to fit onto the nasal canthi.

Reference and Ground Electrodes
Any ophthalmic electrophysiology test recorded on a human requires the use of three electrodes to record the active and reference signals as well as one for ground. The choices for reference and ground electrodes are far less complicated than for active electrodes.
Reference electrode
Reference electrodes serve as a “reference” for ambient biological noise. These electrodes are placed further away from the source of interest on non-stimulated areas. The reference signal is then subtracted from the active signal. The fellow eye may be used as a reference in the event of monocular stimulation. When not using fellow eye as reference, gold cup electrodes are most often used.
Diagnosys highly encourages choosing one method and staying with it so that electrodes are consistently placed because consistent placement equals consistent results.
ERG reference
Options for ERG reference electrode locations include the temple, ear lobe, and fellow eye. Temple locations are most common. Ear lobes are viable, but require more skin prep and cleaning. The fellow eye is optimal, but can only be used during monocular stimulation.
Ear clip electrode
D205 & D210: order here

VEP & EOG reference
VEP reference locations should follow the ISCEV Standard. EOG electrodes placed next to the nasal and temporal canthi act as an active/reference pair.
Ground electrode
A ground electrode serves as the zero reference. The polarity of the recorded voltage is positive or negative relative to ground.
Per ISCEV guidelines, ERG and EOG ground is usually center of forehead, while ground for the VEP is usually centered on top of head. When recording a simultaneous ERG and VEP, the reference electrode will usually be the center of the forehead and ground will be centered on top of head. Although not common, wrist electrodes can also be used for ground.
Wrist electrode
D207 & D230: order here

Electrodes most commonly recommended by Diagnosys
All the electrodes highlighted in this article are commercially available and capable of conducting electrophysiology tests that meet ISCEV guidelines. To assist the researcher or clinician in being able to choose whichever electrode they wish to use, Diagnosys designs all their systems to work with any non-proprietary electrode that uses the industry standard 1.5 mm touch proof connector (known as DIN 42802-1).
Diagnosys recommends the following three electrodes
- DTL Plus
- Gold Cups
- Oval shaped disposable 20x15mm skin electrodes
References
Arden GB, Carter RM, Hogg C, et al. A gold foil electrode: extending the horizons for clinical electroretinography. Invest Ophthal Vis Sci 1979 (April): 421-426.
Bach M, Ramharter-Sereining A. Pattern electroretinogram to detect glaucoma: comparing the PERGLA and the PERG ratio protocols. Doc Ophthalmol(2013) 127:227–238.
Brouwer AH, de Wit GC, de Boer JH, van Genderen MM. Effects of DTL electrode position on the amplitude and implicit time of the electroretinogram. Doc Ophthalmol 2020: 140:201-209.
Dawson WW, Trick GL, Litzkow CA. Improved electrode for electroretinography. Invest Ophthal Vis Sci 1979 (Sept): 988-991.
Esakowitz L, Kriss A, Shawkat F. A comparison of flash electroretinograms recorded from Burian Allen, jet, c-glide, gold foil, DTL, and skin electrodes. Eye1993; 7:169-171.
Hawlina, M, Konec, B. New noncorneal HK*-loop electrode for clinical electroretinography. Doc Ophthalmol 1992; 81:253-259.
Hebert M, Vaegan, Lachapelle P. Reproducibility of ERG responses obtained with the DTL electrode. Vis Res 1999; 39:1069-1070.
Heckenlively JR, Arden GB. 2006 Principles and Practices of Clinical Electrophysiology of Vision 2nd Ed. Cambridge MA, MIT Press.
Hennessy, M. Vaegan. Amplitude scaling relationships of Burian-Allen, gold foil and Dawson, Trick and Litzkow electrodes. Doc Ophthalmol 1994; 89:235-248.
Hidajat RR, McLay JL, Elder MJ, et al. A comparison of two patient-friendly ERG electrodes. Australas Phys Eng Sci Med 2003; 26 (1):30-34.
Kappenman ES, Luck SJ. The effects of electrode impedance on data quality and statistical significance in ERG recordings. Psychophysiology 2010; 47(5):888-904.
Komaromy AM, Brooks DE, Dawson WW, et al. Technical issues in electrodiagnostic recording. Vet Ophthalmol 2002; 5:85-91.
Kurtenback A, Kramer S, Strasser T, et al. The importance of electrode position in visual electrophysiology. Doc Ophthalmol 2017; 134:129-134.
Lapkovska A, Palmowski-Wolfe AM, Todorova MG. Comparing DTL microfiber and Neuroline skin electrode in the mini ganzfeld ERG. BMC Ophthalmology2016; 16:1-37.
Kuze M, Uji Y. Comparison between Dawson, Trick, and Litzkow electrode and contact lens electrodes used in clinical electroretinography. Jpn J Ophthalmol 2000; 44:374-380.
Man TTC, Yip YWY, Cheung FKF, et al. Evaluation of electrical performance and properties of electroretinography electrodes. Trans Vis Sci Tech. 2020; 9(7):1-45.
McCulloch DL, Van Boemel GB, Borchert MS. Comparisons of contact lens, foil, fiber and skin electrodes for pattern electroretinograms. Doc Ophthalmol1998; 94:327-340.
Mohidin N, Yap MKH, Jacobs RJ. Electrodes for multifocal electroretinography (mfERG): a comparison of four electrodes types. Sains Malaysiana 2014; 43(7):1089-1094.
Robson AG, Nilsson J, Li S, et al. ISCEV Guide to Visual Electrodiagnostic Procedures. Springer 2018;136:1-26.
