What is the FST?
The Full-Field Stimulus Test (FST) is a psychophysical test with distinct advantages over other tests for quantifying vision in individuals with advanced retinal degeneration. At its core, the FST assesses visual field sensitivity by determining the lowest luminance flash, eliciting a visual sensation the patient perceives. The test may be done in dark or light-adapted conditions.
The FST: Advancing Ophthalmic Diagnosis for Inherited Retinal Disease
As advances in treatment for Inherited Retinal Diseases (IRDs) progressed, a standard method to quantify extremely low visual perception also needed to progress. In the early 2000s, researchers at the Department of Ophthalmology, Scheie Eye Institute, University of Pennsylvania advanced the FST to a level that made it possible to effectively quantify the lowest levels of visual perception (Jacobson et al, 2007).
Recognizing the potential for the FST to evaluate novel IRD treatments, leading pharmaceutical companies approached Diagnosys to design the software and hardware for a commercial FST platform. Diagnosys along with its consultant Professor John Robson, ScD FRS designed a radical new style of psychophysical FST that was faster, more accurate, and more reproducible than previous FST methods.
The DiagnosysFST® tests patients with algorithmically derived flash luminance levels to which they must answer YES or NO on a two-button box in response to whether or not they saw the stimulus. Requiring the individual to positively indicate NOT seeing the stimulus is a unique feature in psychophysical testing. In addition, the DiagnosysFST® not only provides a quantified measure of the patient’s light perception threshold but also automatically implements a quality metric scoring system to simplify data interpretation.
Spark Therapeutics developed Luxturna®, the first FDA approved gene therapy treatment. Luxturna® is a treatment for Leber’s Congenital Amaurosis caused by a mutation of the RPE65 gene. Spark used DiagnosysFST® throughout the research and development phases. Now, Novartis is using this test to measure the efficacy of the Luxturna® treatment.
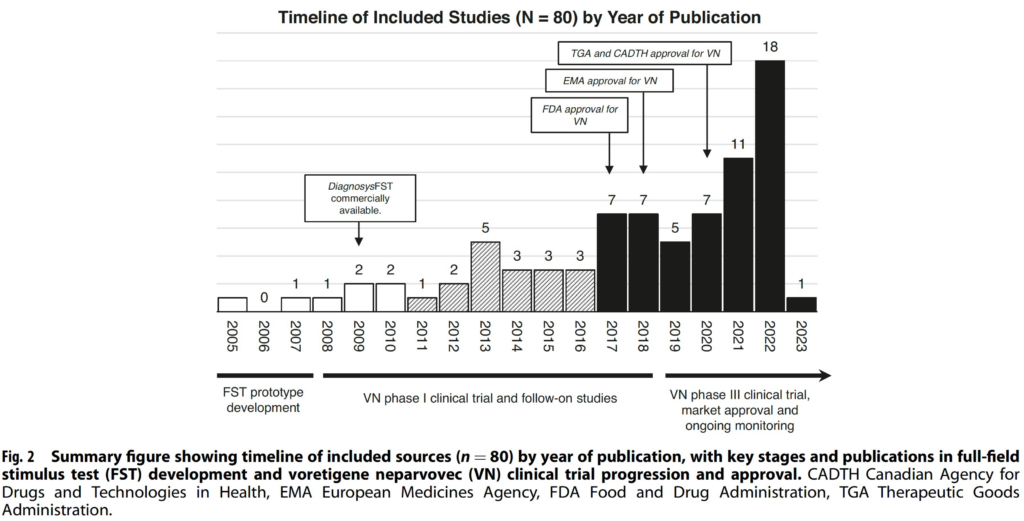
The following chart shows the timeline for government approval of Luxturna® in the US, Europe, Australia and Canada (Thompson et al 2023).
Is FST an appropriate test for your application?
A comparison to Dark Adaptometry, Visual Fields, ERG, and VEP
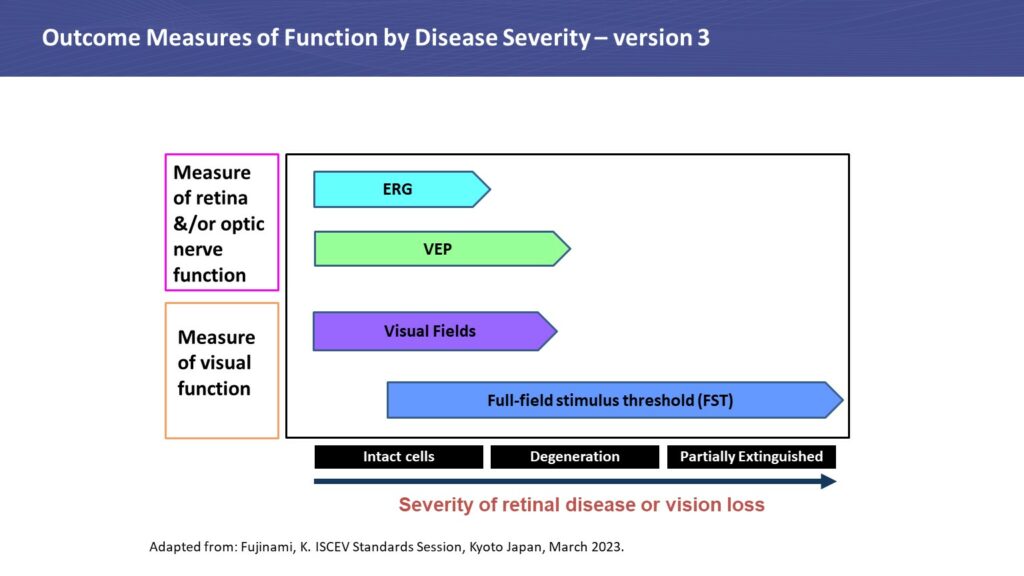
The following chart indicates the capability of these tests in relation to each other. Please note that Dark Adaptometry is not on the chart but covers the same range as FST. However, DA is a significantly longer test and is seldom used for low vision patients.
Dark Adaptometry (DA)
Like the FST, DA is a psychophysical test. It assesses an individual’s ability to adapt to darkness, much like what a person experiences when walking into a dark room after being outside in the bright sunlight. The classic DA procedure is predicated on the Goldmann–Weekers dark adaptometer which uses a
full-field stimulator with a white-coated interior to present an 11-degree target, 11 degrees inferior to fixation. Following 4 to 5-minute adaptation to a bright uniform field (bleaching), an ascending method of limits is used to determine the patient’s response during a 20–40 min period of DA testing (Rabin et al, 2017).
The patient is tested while they are dark adapting throughout the 20-40 minutes and must respond to flashes of light by pushing a single button box if light is seen. A staircase method for choosing flash luminance is the preferred option for DA because the individual is constantly dark adapting throughout the test. The staircase method makes it practical to find the threshold, which is a moving target during many periods of the test.
As indicated by the name, dark adaptometry is a scotopic test and it is usually done monocularly. In the case of a full-field test, the individual does not have to fixate. In the case of the Goldmann-Weeker test, there is a target and the patient will need to fixate. At the end of the test, the fully dark-adapted threshold is measured and recorded.
There are several retinal diseases that can prolong the time required to adapt to darkness, as well as the level of sensitivity achieved at any point during the test. Thus, DA can be an important test for accurate diagnosis of retinal disease such as age-related macular degeneration while also for providing invaluable guidance for patients with impaired night vision.
Visual Field (VF)
Visual field is the name for the entire area that you can see. This test measures how sensitive your vision is in different parts of your visual field. It also measures your peripheral vision, that is how well you can see above, below, and to the sides when you are looking straight ahead.
Like FST and DA, VF is a psychophysical test requiring the patient to report a visual sensation to a stimulus by pushing a single-button box when light is seen during the test.
Several basic conditions must be met for the test to successfully map the visual field. The individual must be able to maintain a constant gaze toward a fixed location for several minutes. Each eye is tested separately, while the opposite eye is covered with a patch. Refractive correction must be made with a test lens. Spectacles must not be worn because they can cause false defects in the visual field due to their shape. In addition, corrections must be made for presbyopia to reduce accommodative strain (Carroll and Johnson). The VF test is often 5-10 minutes long.
The most widely used VF test is the Humphrey Visual Field (HVF) because it is automated, often using the Swedish Interactive Thresholding Algorithm (SITA). SITA is a forecasting procedure that uses Bayesian statistical properties similar to the methods used for providing weather information and predictions. SITA allows for more rapid analysis than would be possible without forecasting. By considering a user’s results in nearby locations, stimuli that are unlikely to be seen or extremely likely to be seen are rarely tested. Instead, the stimuli that are likely near threshold are tested. (Carroll and Johnson)
There are several common protocols based on the purpose of the test:
• 10-2: Measures 10 degrees temporally and nasally and tests 68 points.
• 24-2: Measures 24 degrees temporally and 30 degrees nasally and tests 54 points.
• 30-2: Measures 30 degrees temporally and nasally and tests 76 points.
The first number denotes the extent of the field measured on the temporal side, from the center of fixation, in degrees. The larger the number, the more general the screening. The ‘-2’ represents the pattern of the points tested. Stimuli will vary in size and intensity.
Prior to HVF, there was the Goldmann Visual Field test (GVF). This method is not as widely used because it requires skilled perimetrists to manually map the visual field without the aid of a computer algorithm like SITA.
A VF test will provide more localization of visual impairment than either the FST or DA, however it is a test that can be challenging for patients who are unable to fixate or concentrate, and is especially difficult if not impossible for low vision patients.
Electroretinogram (ERG)/ Visually Evoked Potential (VEP)
Unlike FST, DA, and VF, the ERG and VEP are not psychophysical tests. Both use electrodes placed in various positions on the scalp and on/near the eye in order to directly measure the electrical response of components in the visual system to a stimulus. Patients do not need to push any buttons to report a visual response.
For low vision patients, ERGs/VEPs are often flat because the electrical signal is too small to be detected by even the best amplifiers. However, in most cases even though the ERG/VEP is flat, visual perception is still occurring and is still quantifiable.
Unveiling FST’s Versatility
The wider ophthalmic community is beginning to recognize the versatility of the FST. While primarily known as a full-field test, with proper equipment the FST has the option of being a partial-field test. It is a monocular test for both scotopic and photopic testing and does not require the patient to fixate. The FST is also a quick test. Once the patient is adapted, testing time is only 1-2 minutes per test. Bleaching is not necessary. The array of stimulus colors—red, green, blue, amber, white—further enhance its versatility. For photopic tests, all colors can be used for flash or for background. White, blue, and red are most common for scotopic tests. Currently, a mesopic version of FST is in development.
Conclusion
As described above, the FST has a distinct advantage over other tests for quantifying vision in individuals with advanced retinal degeneration. To address the challenges inherent in a psychophysical test, DiagnosysFST® incorporates unique features such as the two-button box, a pseudo random luminance selection algorithm, and a built-in quality scoring mechanism that sets it apart from other testing platforms, a statement confirmed by a recent review of 80 FST applications (Thompson et al 2023). All 80 publications used DiagnosysFST®.
References
Roman AJ, Cideciyan AV, Aleman TS, Jacobsen SG. Full-field stimulus testing (FST) to quantify visual perception in severely blind candidates for treatment. Physiol. Meas. 28 (2007) N51–N56.
Rabin J, Houser B, Talbert C, Patel R. Measurement of dark adaptometry during ISCEV standard flash electroretinography. Doc Ophthalmol (2017) 135:195–208.
Shi LF, Hall AJ, Thompson DA. Full-field stimulus testing: a scoping review of current practice. Nature (2023) Eye; https://doi.org/10.1038/s41433-023-02636-3
Carroll JN, Johnson CA. Visual Field Testing: From One Medical Student to Another. The University of Iowa Department of Ophthalmology and Visual Sciences. https://eyerounds.org/tutorials/VF-testing/

